Treatments
Different approaches
An abdominal surgeon performs surgical procedures in the abdomen (= the belly).
In the next chapters we discuss the most frequently performed surgical procedures performed in the abdomen. Because every operation has a big impact on the well being of the patient we think that clear information and an honost relation between patient and surgeon is of great importance.
For abdominal surgery different approaches are used which are discussed briefly below.
There is a big difference between an open approach or minimal invasive surgery (MIS).
Open approach
With an open approach the operation is started by making a small or bigger incision to get a view on the target area. This approach is sometimes preferred for more complex procedures or if tactile feedback is crucial and the touch of the hands is needed.
This is also often the case for redo surgery in the abdomen (history of several abdominal procedures) or when a bigger mass/tumor has to be removed.
Laparoscopy (MIS)
In most procedures MIS is more elegant because the incisions are much smaller. Because of the smaller incisions the postoperative pain is less which results in faster mobilization of the patient and reduced impact on breathing and coughing. As a result in most cases the patient recovers in a more elegant way. Also the risk of surgical site infections is less.
In minimal invasive surgery (MIS) we distinguish laparoscopy from robotic surgery.
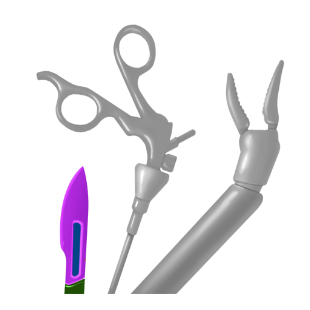
During laparoscopy an assistant is holding the camera while the surgeon performs the procedure with specially designed instruments through small working trocars. The whole team is performing the procedure while watching on a TV-screen having a 2D-image. A well trained laparoscopic surgeon knows the relation between the anatomical structures and “knows” the third dimension.
Robotic surgery (MIS)
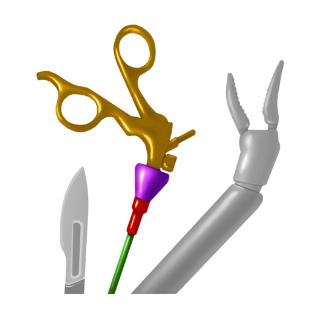
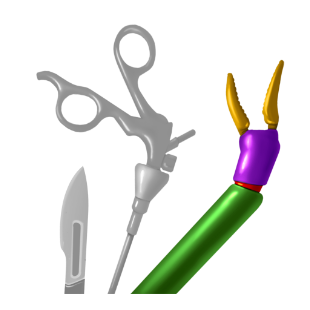
The incisions for robotic surgery are comparable to laparoscopic surgery, but the surgeon is working from a console which is connected to the robotic arms. With control pedals the surgeon can control the robotic arms and the camera which has a 3D view. There is a possibility to zoom in and out. Probably some surgical procedures can be performed even more precise than in laparoscopy although this was never confirmed in large clinical trials.
For now the robot is mainly used for procedures in which a stable 3D image is wanted and where the possibility to zoom in is important, especially for locations that are hard to reach during laparoscopic procedures.
Prof. Joep Knol performs all three approaches, but with a focus on MIS.
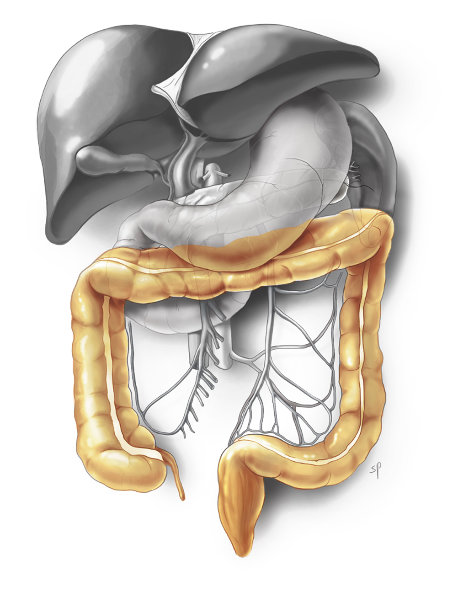
The colon and rectum are shown in orange
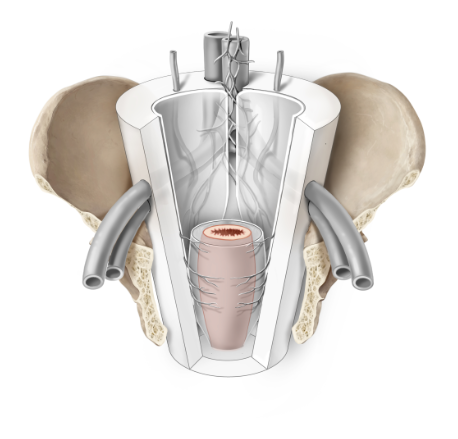
Rectal cancer surgery is more difficult because of working in a funnel shaped pelvis.
Colorectal
In general, diseases of the colon ( = large bowel) can be classified in 4 groups:
1. Tumors of colon and rectum
2. Acute inflammatory diseases
3. Chronic inflammatory diseases
4. Functional diseases
For all these diseases of the colon and rectum a multidisciplinary approach is needed to guarantee best treatment for the patient. In general an operation is only the last option if more conservative treatment is failing. Of course there are some diseases that can not be classified in one of the groups above.
Tumors of colon and rectum
Tumors can be benign or malignant (= cancer). Colorectal cancer is the third cause of death by cancer, despite a declining incidence in relation with the detection of early lesions (polyps) by screening with colonoscopy (National Screening Programms). Optimally a benign lesion is found before it advances to a malignancy. However, a significant number of patients present with metastatic disease (liver, lungs) at the time of presentation.
Treatment
Surgery is the cornerstone of treatment of colorectal cancer.
For all surgical procedures the key thing is to remove the cancer together with the fatty tissue that contains draining vessels and lymph nodes along which tumor cells can potentially disseminate. For the colon we call this area the mesocolon, for the rectum we call this mesorectum. The quality of surgery is determined by the compleness of removal of this mesocolon/rectum.
Although every operation has a certain risk for infectious complications, for colorectal surgery there is a specific risk for anastomotic complications after restoring bowel continuity. When an anastomotic leakage appears in most cases a reintervention is needed.
In 90% of cases these procedures are performed by a minimal invasive (laparoscopic or robotic) approach. On average these procedures take about 2-3 hours to perform depending on location in the abdomen and extent of the lesion. Hospital stay is 3-5 days in most cases.
After recovering from the operation in some cases adjuvant chemotherapy is needed, depening on the tumor stage and lymph node invasion by cancer cells.
Rectal cancer surgery is more complex because of limited manoeuvrability in the funnel shaped pelvis. On the side of the pelvis, important vessels and nerves should be preserved as much as possible because they play an important role in “pelvic happiness” (cfr Professor Bill Heald) which is sexual, bladder and bowel function. Also, for very low located lesions a judgement has to be made whether to preserve the sphincter muscle without limiting the oncologic outcome and still with an adequate functional result. As a result rectal cancer surgery is more complex and requires specific training for the surgeon. By combining minimal invasive surgery with transanal surgery (more info in “Thesis”) more sphincters can be preserved with more adequate judgment of the lower border of the cancer. Patients should be selected for this combined procedure (especially obese patient with low lesions in a very narrow pelvis) and additional training is needed for the surgical team.
Joep Knol is considered an expert for this procedure; he trained surgeons around the globe and published many manuscripts on optimal training of the procedure.
Rectal cancer surgery takes about 3-6 hours and requires a 5-7 days hospital stay.
Acute inflammatory diseases
The most frequent causes of acute inflammatory disease of the colon are appendicitis and diverticulitis.
Appendicitis
Appendicitis is a painful swelling of the appendix. The appendix is a small, thin pouch of about 5-10 cm. long. It’s connected to the large intestine and located on the right side of the abdomen. You can get appendicitis at any age, but it usually affects young people aged between 10 and 20 years.
Appendicitis typically starts with a pain in the middle of your abdomen that may come and go. Within hours, the pain travels to the lower right-hand side, where the appendix usually lies, and becomes constant and severe. Pressing on this area, coughing or walking may make the pain worse. The patient may have fever, lose apetite and feel sick.
There may also be a less typical course so to diagnose appendicitis is not always that easy.
In some cases an appendicitis can be treated with antibiotics, but in most patients an appendectomy (removal of the appendix) has to be performed. An appendectomy is most frequently performed by laparoscopy. With laparoscopy, smaller incisions are made and the entire abdomen can be checked for other causes of abdominal pain; recovery is a bit faster as well. The risk of surgical site infections is reduced.
An appendectomy takes about 30-60 minutes and requires a 1-3 days hospital stay.
In some cases prolonged administration of IV antibiotics is required.
Diverticulitis
Diverticulitis is a painful swelling of diverticula (small pouches) of the colon, most frequently the sigmoid, located on the left side of the abdomen. More than 50% of individuals aged > 60 have diverticula, yet the vast majority have no or minimal symptoms. If symptoms appear it resembles a “left appendicitis”. Pressing on this area, coughing or walking may make the pain worse. The patient may have fever, lose apetite and feel sick.
Bleeding and pain in the lower left part of the abdomen (diverticulitis) may occur and requires medical evaluation with CT scans and colonoscopy to establish the diagnosis and assess disease location and severity. Non-complicated diverticulitis is treated with oral antibiotics, while complicated (abscess, peritonitis) diverticulitis is a more severe presentation which justifies inpatient management with IV antibiotics, drainage and/or emergent surgery.
Treatment
During the surgical procedure the sigmoid is removed after which bowel continuity is restored (in most elective cases) or an ostomy is required (in most emergent cases or if complications appear).
An elective laparoscopic sigmoid resection requires 4-5 small skin incisions (5-10 mm), takes about 90 minutes and requires a 3-4 days hospital stay. The course after an emergent operation is less predictable and hospitalization can take longer.
Chronic inflammatory diseases
Crohn’s disease and Ulcerative Colitis are chronic inflammatory diseases (IBD = Inflammatory Bowel Diseases). While Crohn’s disease can appear in the entire gastrointestinal tract, Ulcerative Colitis is restricted to the colon and rectum.
In both diseases medical treatment has priority. A surgical procedure is only indicated when medical treatment fails or when complications appear. An operation consists in most cases of removal of (a part of) the bowel.
Functional diseases
With functional diseases of the colon and rectum we consider functional disorders like dyschezia, constipation or incontinence.
Dyschezia is the difficulty in defecating, sometimes as a result of prolaps. Constipation is irregular and infrequent or difficult evacuation of the bowels. Incontinence is the unability to voluntary control defecation.
Surgery is only the last option and even then normal function will not be reached but quality of life can be improved.
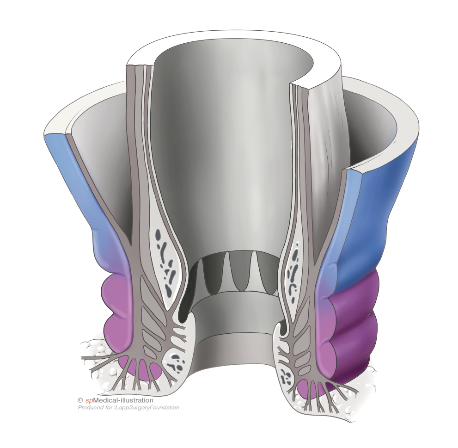

Proctology
Diseases of the anus and anal canal are quite common in individuals of all ages.
Most frequent problems are:
- Hemorrhoids
- Fissures
- Abscesses
These problems have their own typical course and symptoms which allows us to differentiate even before a clinical exam. All diseases can cause pain, bleeding and discomfort though.
A gentle but thorough clinical examination by a specialist is mandatory to make a diagnosis and exclude life-threatening conditions, such as anorectal cancer and perineal sepsis.
Treatment
Peri-anal abscesses require emergency surgery to evacuate the pus and drainage of the residual cavity. Pressure and pain will be releaved after this procedure.
Fissures are treated with laxatives and pomades in most cases. Sometimes an operation is required. Hemorrhoids with mild symptoms can be treated by infrared treatment, Barron ligatures or sclero-injections. Prolapsed hemorrhoids with severe symptoms are an indication for surgery.
Because the skin of the anus has a lot of nerves, operations are sometimes painful especially if a resection of the skin itself is necessary.
Most surgical procedures are performed in an ambulatory setting, take less than 30 minutes, and usually require 7-10 days sick leave.

Sleeve gastrectomy
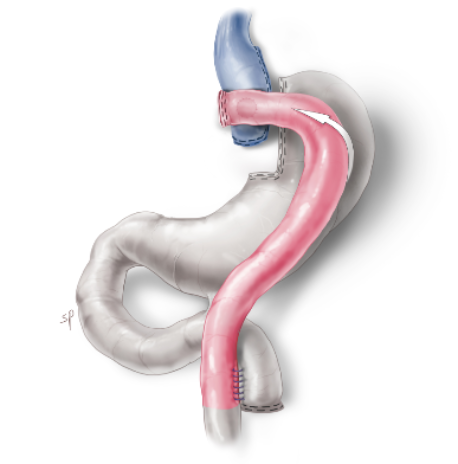
Gastric bypass
Obesity
In Belgium two groups of people are candidates for bariatric surgery,
- Morbid Obesity (BMI > 40 kg/m2)
- Severe Obesity (BMI > 35 kg/m2) + 1 or more complications related to obesity (diabetes, high blood pressure treated with medication, sleep apnea, former failed bariatric surgery)
A multidisciplinary approach is necessary and crucial for both a good result and healthy weight reduction. A lifelong intake of vitamins and calcium is crucial.
Patients have to be very disciplined throughout the rest of their lives.
Weight loss surgery offers the obese patients an opportunity to lose 50-75% of their excess weight (excess weight = current weight – ideal body weight), but may also cure associated diseases, such as diabetes and sleep apnea.
Treatment
Dr. Joep Knol performs bariatric surgery for more than 15 years.
He works in a multidisciplinary team led by the coordinating nurse of the Obesity Clinic.
Both the Sleeve gastrectomy (see first illustration) and Gastric bypass procedure (see second illustration) are performed by laparoscopy.
These procedures are performed using 4-5 small incisions, take about 60 minutes to perform and require a 1-2 days hospital stay.


Reflux
Gastroesophageal reflux disease (GERD) is a common problem, which affects 20% of the adult population. Once the diagnosis is established by the gastroenterologist, lifestyle modifications (weight loss) and medical treatment (proton pump inhibitors, such as omeprazole) is introduced.
For those patients who fail to respond to this conservative approach, who have side-effects of PPI’s, or who present with large hiatal hernias, the indication for surgery should be discussed by a multidisciplinary team.
Treatment
The best surgical option in thin patients is a laparoscopic Nissen fundoplication, which consists in wrapping the upper part of the stomach around the lower esophagus.
This wrap works like a valve and reduces reflux of acid.
Laparoscopic gastric bypass is the procedure of choice when morbid obesity (BMI > 40 kg/m2) and GERD coexist. In this case there will also be counseling by the bariatric team.
Both procedures are performed with a minimally-invasive approach using 4-5 small (1cm) incisions, and require a 1-3 days hospital stay.
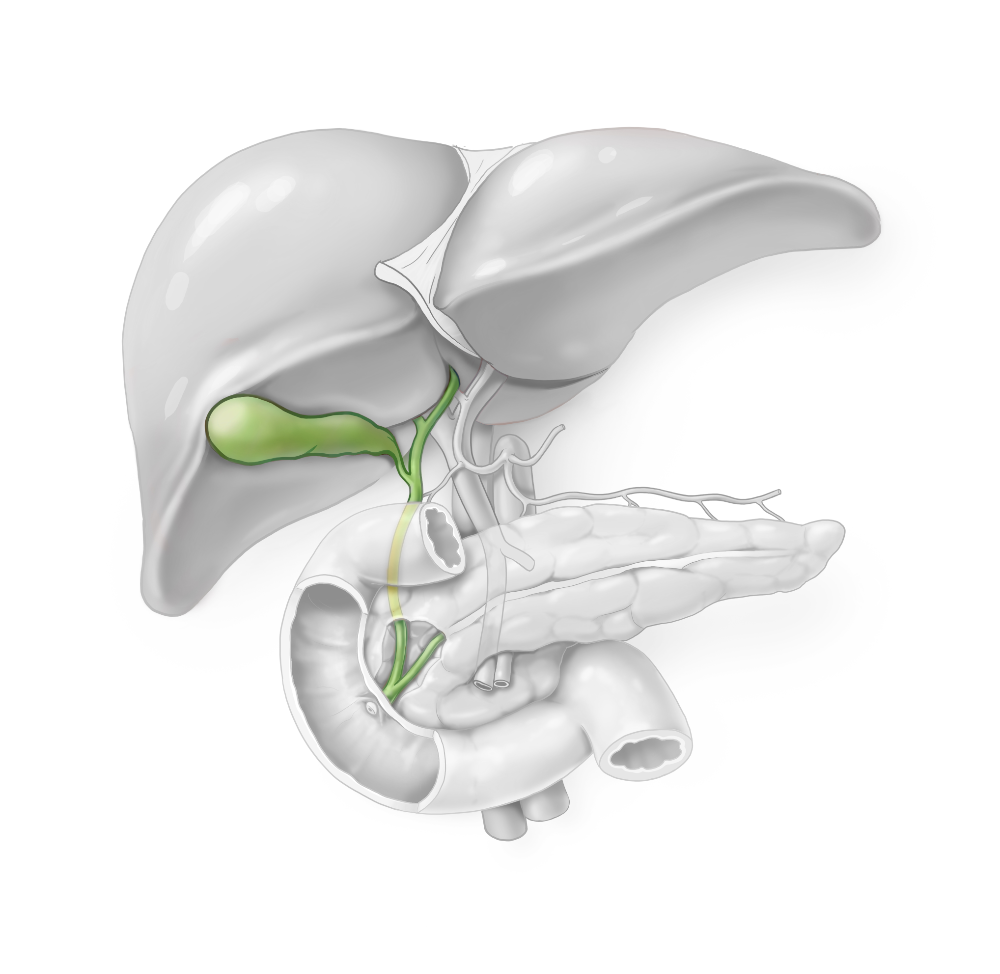
Gallstones
The gallbladder is a small pouch located at the inferior face of the liver, which is responsible for stocking bile between meals. The liver produces around 1 liter bile a day.
When food enters the stomach and duodenum, the gallbladder contracts and about 100mL of bile is excreted in the bowel, primarily for helping to digest fat.
Due to an inbalance of cholesterol and bile pigments, little cristalls can be formed in the gallbladder which can enlarge and become stones. Depending on the constitution of the stone we can differentiate cholesterol stones, pigment stones and mixed stones.
A lot of adults have gallstones, but many of them are asymptomatic.
Symptomatic gallstones are more frequently present in female patients around 40 years with fair hair. So FFF: Female, Forty, Fair.
Typical symptoms are repeated abdominal colicky pain (sever pain in the middle to right upper abdomen often occurring after eating a heavy meal), jaundice (yellowish tinge to skin and eyes), inflammation of the gallbladder (cholecystitis), and inflammation of the pancreas (pancreatitis) or the main bile ducts (cholangitis).
The worst pain of biliairy colic commonly lasts for 30 minutes to an hour, but may continue at a lower intensity for several more hours. The pain stops when the gallstone breaks free of the bile duct and passes into the intestine.
Treatment
Gallstones, when they are responsible of symptoms, are an indication for surgery. The operation consists of removing the gallbladder (laparoscopic cholecystectomy) and the stones, through a minimally invasive technique with 4 incisions of 5-10 mm.
The procedure takes about 1 hour to perform and the patients usually stay in the clinic for 0-1 nights.


Hernia
A hernia is a protrusion of the abdominal content through a weak spot of the abdominal wall.
This weak spot can be the result of a former operation/scar, but also due to some natural weak spots. The umbilicus is a natural weak spot due to the umbilical cord we had at birth, and also the inguinal region is a weak spot especially in male patients because the testicles have to migrate into the scrotum after birth. Along this course an inguinal hernia can appear early or later in life.
Hernias can cause significant discomfort, and in a minority of cases can lead to complications such as bowel occlusion. Discomfort or the risk for complications is an indication for surgery.
It is a mechanical problem more than a disease, and there is no therapeutic alternative to surgery.
Treatment
Surgical treatment is curative, and nowadays performed with mesh placement.
For an inguinal hernia we sometimes perform open surgery with tension-free reinforcement of the inguinal floor (Lichtenstein repair). For this procedure an incision of 4-7 cm. has to be made after which the hernia is reduced and a mesh can be placed. As an alternative it’s very elegant to perform a minimal invasive procedure for which 3 small incisons of 0.5-1.5 cm. have to be made for both a unilateral and bilateral repair. The mesh will be placed in the extra-peritoneal space (TEPP repair).
Umbilical and other small hernias are treated with a small incision at the location of the hernia. For each individual one has to decide whether to use a mesh or not.
Larger hernias are more difficult to repair and require larger meshes. The repair can be done by an open or minimal invasive approach. Because the robot has the option to look down to up (“towards the ceiling”) in selective cases the use of it is a good alternative.
Small hernias can be repaired during an ambulatory (outpatient) or short (1 night) hospital stay according to patients’ age, social status and co-morbidities. Repair of larger hernias sometimes requires a hospital stay of 3-5 days.
